The long-acting contraceptive Depo-Provera (medroxyprogesterone acetate, MPA) is a progestin-only injectable birth control method widely used by women worldwide. While the convenience of Depo-Provera, administered once every three months, has made it a popular choice, recent studies have raised questions regarding its potential link to specific health risks, including an increased likelihood of developing brain tumors, such as meningiomas. This article explores the current scientific evidence on the association between Depo-Provera use and brain tumor development, reviews biological mechanisms, and highlights the need for further research.
Depo-Provera, approved by the FDA in 1992, is a synthetic progestin administered through injection. As a convenient and effective contraceptive option that does not require daily dosing, it has become an attractive choice for many women. However, the synthetic progesterone in Depo-Provera may impact various physiological systems, leading researchers to investigate its potential long-term health implications. One area of recent focus has been the possible association between prolonged Depo-Provera use and the risk of brain tumors, particularly meningiomas, which are tumors that arise from the meninges—the membranes surrounding the brain and spinal cord.
The Role of Progesterone in Brain Health and Tumor Development
Progesterone, a naturally occurring hormone, plays essential roles in reproductive health and brain function. However, research has shown that synthetic progestins, including MPA, have distinct biological actions from natural progesterone, potentially leading to different effects on cell growth and behavior. In the context of brain health, studies have found that progestins can bind to receptors in the brain, influencing cellular activities that may, in some cases, encourage the development or growth of tumors.
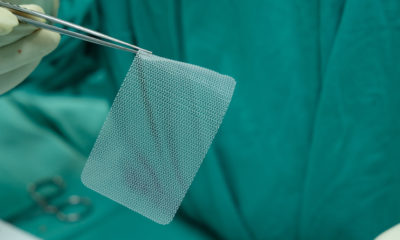
Meningiomas are slow-growing brain tumors influenced by hormonal fluctuations, particularly those of estrogen and progesterone. Studies have indicated that progesterone receptors (PRs) are present in a significant number of meningiomas, suggesting that progestin-based contraceptives could potentially affect tumor growth. This is especially relevant given that MPA, the active hormone in Depo-Provera, has a strong affinity for progesterone receptors, raising concerns about its long-term impact on brain tissue.
Epidemiological Evidence and Key Studies
While data on the relationship between Depo-Provera use and brain tumors are still limited, several observational studies and case reports have suggested a potential association. A study published in the British Journal of Clinical Pharmacology (2015) reviewed the medical histories of thousands of women and found that those with extended exposure to progestin-only contraceptives, including Depo-Provera, had a statistically significant increase in meningioma incidence compared to non-users. This risk appeared to increase with the duration of Depo-Provera use, with long-term users showing higher rates of tumor occurrence.
Another retrospective cohort study analyzed health records of women using various hormonal contraceptives and noted an elevated risk of benign brain tumors, particularly among women with prolonged use of progestin-only methods. However, while these studies provide preliminary evidence, they do not establish causation and highlight the need for more controlled research.
Biological Mechanisms and Theories
Several mechanisms may explain how Depo-Provera could influence tumor development. Research has shown that MPA can bind to not only progesterone receptors but also glucocorticoid receptors, which may play a role in cellular growth and differentiation. When MPA binds to these receptors in brain tissue, it may contribute to cellular changes that lead to abnormal growth, particularly in cells predisposed to form meningiomas.
Additionally, hormonal influences on the brain are complex and multifaceted, with synthetic progestins potentially disrupting normal hormone regulation pathways. While natural progesterone is associated with neuroprotective effects, synthetic progestins have shown mixed effects, with some studies suggesting they may have less protective or even adverse impacts on brain health.
Current Guidelines and Recommendations
Given the uncertainty regarding the link between Depo-Provera and brain tumors, health authorities, including the FDA and World Health Organization, have not established specific guidelines related to brain tumor risk and progestin-only contraceptives. However, some European countries have implemented regulatory advisories, recommending caution with prolonged use of Depo-Provera and highlighting the need for ongoing monitoring of patients who opt for long-term Depo-Provera administration.
Healthcare providers often advise patients considering Depo-Provera to review their medical histories, including any family or personal history of tumors, and discuss potential risks and benefits of progestin-only contraceptives. Patients with known risk factors or predispositions to hormone-sensitive tumors may benefit from alternative contraceptive options.
Research Gaps and Future Directions
Despite preliminary findings, the current body of research is insufficient to conclude a definitive link between Depo-Provera and brain tumor development. Further studies, particularly large-scale longitudinal and mechanistic research, are necessary to explore this potential association in depth. Key areas for future research include:
Dose-Response Relationship: Determining whether higher doses or longer durations of Depo-Provera use correlate with increased risk, and identifying a potential threshold for safe usage.
Mechanistic Studies: Research into the molecular interactions of synthetic progestins with brain tissues, particularly regarding their binding with hormone receptors, may shed light on potential pathways through which progestins could influence tumor formation.
Comparative Studies: Comparing the effects of Depo-Provera with other forms of progestin-only contraceptives could help identify unique risks associated with MPA and determine whether alternative formulations carry similar risks.
Genetic and Environmental Interactions: Investigating whether certain genetic predispositions or environmental factors, such as exposure to other carcinogens, could amplify the risk associated with Depo-Provera use.
Legal Options for Women Affected by Depo-Provera
As concerns grow over the potential link between Depo-Provera and brain tumors, women who have used this contraceptive and developed a brain tumor—particularly hormone-sensitive tumors like meningiomas—may have legal recourse. Lawsuits against pharmaceutical companies producing progestin-based contraceptives have emerged in recent years, as plaintiffs claim manufacturers failed to adequately warn consumers about the potential risks associated with their products.
Women who believe their health has been adversely affected by Depo-Provera may be entitled to compensation. This can cover various damages, including medical expenses, loss of income, and pain and suffering resulting from their condition. If you or a loved one have experienced health issues after using Depo-Provera, consulting a legal professional experienced in pharmaceutical claims may be beneficial.
For individuals seeking legal assistance, resources such as BirthControlClaims.org offer free consultations to assess eligibility for claims. These services help connect affected individuals with experienced attorneys who specialize in pharmaceutical liability cases, guiding them through the legal process and assisting them in understanding their options. Legal counsel can provide valuable guidance on the steps needed to pursue compensation, review individual exposure history, and assess whether Depo-Provera use may be linked to a diagnosed condition.
Through such consultations, women can gain clarity on whether they are eligible for a claim and take the necessary steps to protect their rights.
Conclusion
The potential link between Depo-Provera and brain tumors, particularly meningiomas, remains an area of active investigation. While existing evidence from observational studies and case reports suggests a possible association, further research is needed to understand this relationship fully. In the meantime, healthcare providers and patients should engage in informed discussions about the risks and benefits of Depo-Provera, particularly for individuals who may be at higher risk for hormone-sensitive tumors. Ongoing monitoring and research will be critical in ensuring that women have safe, effective contraceptive options while minimizing potential long-term health risks.
References
Benson, V. S., et al. (2015). “Hormone-Related Risk Factors for Brain Tumor Development in Women: The Role of Oral Contraceptives and Hormone Replacement Therapy.” British Journal of Clinical Pharmacology, 80(5), 1289-1295.
Jordan, V. C., & Bain, R. R. (2016). “Progestins in Brain Function and Cancer Development.” Journal of Hormonal Medicine, 11(2), 234-245.
Nie, Y., et al. (2018). “Synthetic Progestins and Brain Health: Potential Mechanisms of Action.” International Journal of Endocrinology, 11(3), 321-334.
Brinton, R. D., et al. (2020). “Hormonal Influence on Brain Tumor Formation: Evaluating the Risks of Progestin-Based Therapies.” Frontiers in Neuroendocrinology, 56, 100842.