The U.S. Food and Drug Administration issued a statement on January 25, 2019, updating the public on the ongoing investigation into valsartan blood pressure medications that are contaminated with impurities that are probable human carcinogens. The FDA warns that these drugs are in shortage and that other blood pressure medications may also fall into short supply soon.
What is Valsartan
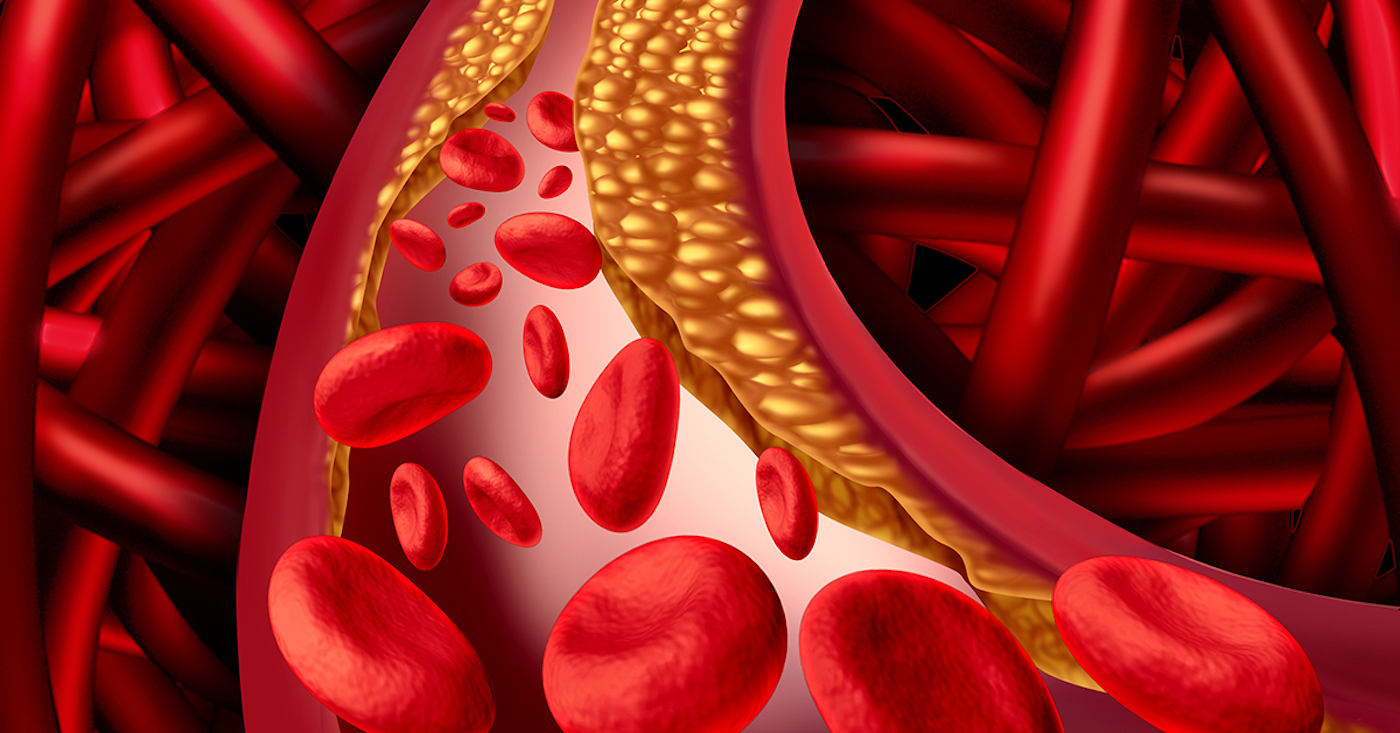
Valsartan is a blood pressure medication that belongs in a class called angiotensin II receptor blockers, or ARBs. Recently, valsartan, losartan, and irbesartan were all recalled from the U.S. market after it determined that these drugs contained an impurity that poses a risk of cancer to patients.
The FDA discovered in July 2019 that some valsartan blood pressure drugs were contaminated with nitrosamine impurities such as N-Nitrosodimethylamine or NDMA, and N-nitrosodiethylamine or NDEA, chemicals deemed possible carcinogens. And while these are environmental contaminants typically found in dairy products, meats, and vegetables, and water, these substances are not acceptable in medications.
According to the statement, the FDA determined the medications were contaminated during the manufacturing process, and the contamination could have come from the reuse of materials like solvents.
How Is the Blood Pressure Medication Tainted?
Some of the ingredients imported from a pharmaceutical company in China were tainted with the impurities, according to the federal watchdog agency. The pharmaceutical company was put on an import alert that will flag all pharmaceutical and finished products to prevent them from entering the U.S. The FDA said it made this decision to flag these products after finding that supervision issues at the pharmacy could have created conditions that allowed the quality issues to occur.
When the FDA determined that ARB medications were tainted with impurities, the agency started gathering samples of all ARB medications and found NDEA in valsartan products made by different manufacturers.
To detect and quantify the amount of NDMA and NDEA in this class of medications, the FDA developed special testing methods including the headspace method, the combined headspace method, and the combined direct injection methods.
What Patients Should Know
As far as exposure to the tainted medications, the FDA said it appears small. However, the agency is working to balance patients consuming low-level impurities over a short period of time with the risk that some ARBs are in short supply and could impact how patients get the medications they need.
Unfortunately, the long-term health implications posed by NDMA are uncertain, as the amount that is consumed is what matters. According to CNN, NDMA is a toxin that, when consumed in large enough doses can cause liver fibrosis and liver tumors in rats. Unfortunately, most of what is known about the potential carcinogen has been determined in animal studies.
FDA scientists estimate in a worst-case scenario that if 8,000 patients consumed the highest valsartan dose for four years, only one additional patient would develop cancer above the average cancer rate for 8,000 people.
Patients who are affected by the short supply of ARB medications should speak with their physician as soon as possible for advice and possible alternative therapies.